Periodontal
Gum Care
Our most recent
digital and strategy projects.
General Dentistry
Periodontal Disease (Gum Disease): Everything You Need to Know
Periodontal disease — often called gum disease — is a progressive inflammatory condition that affects your gums and the underlying bone that supports your teeth. While it can stem from poor oral hygiene, certain people are naturally more susceptible, even if they brush and floss regularly. Left unmanaged, periodontal disease can lead to gum recession, loose teeth and, ultimately, tooth loss. However, early detection and proper treatment can slow or even halt its progression.
How Common Is Periodontal Disease?
Periodontal disease is widespread across different age groups. Research suggests that nearly half of adults have some form of gum disease. It’s also one of the leading causes of tooth loss. Understanding the warning signs and risk factors is critical to safeguarding your oral health.
Symptoms and Warning Signs
Gum disease can advance slowly, and many people don’t experience pain in the early stages. However, you should see a dentist if you notice any of these warning signs:
- Reddish, purplish or swollen gums.
- Gums that bleed easily during brushing or flossing.
- Persistent bad breath (halitosis) or an unpleasant taste in your mouth.
- Sensitivity or pain when chewing.
- Receding gums (making your teeth look longer).
- Loose or shifting teeth.
- Changes in the way your bite feels.
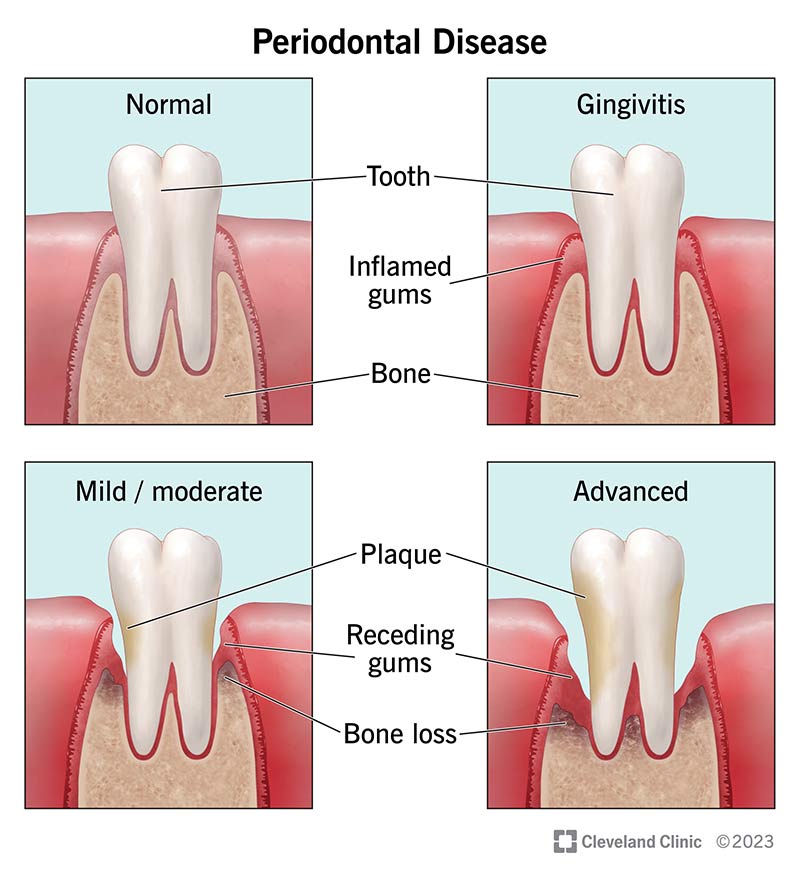
Stages of Periodontal Disease
Periodontal disease progresses in distinct stages, ranging from mild to severe:
- Gingivitis: The earliest form of gum disease. Gums become inflamed, swollen and may bleed when you brush or floss. At this stage, there’s no bone loss, so gingivitis is fully reversible with the correct dental care.
- Mild Periodontitis: Bacteria start penetrating beneath your gum line, forming pockets that collect plaque and tartar. Early bone loss may occur, leading to slight gum recession.
- Moderate Periodontitis: As the infection advances, the supporting tissues and bone around your teeth start to break down more significantly. You may notice bad breath, pus, and increased sensitivity.
- Advanced Periodontitis: This stage is marked by extensive bone loss. Teeth may become very loose or even fall out. Advanced periodontitis often requires comprehensive surgical intervention to manage.
Causes and Risk Factors
The primary culprit of gum disease is plaque buildup — a sticky film loaded with bacteria. If not removed by regular brushing and flossing, plaque hardens into tartar and triggers infection. Additional factors that increase your risk include:
- Poor oral hygiene: Infrequent or inadequate brushing and flossing.
- Smoking or tobacco use: Harms gum tissue and impedes healing.
- Genetics: Some people inherit a predisposition to gum disease.
- Diabetes: High blood sugar can promote bacterial growth.
- Autoimmune conditions: Diseases like lupus or Crohn’s affect your immune response.
- Hormonal changes: Pregnancy, puberty and menopause can lead to heightened gum sensitivity.
- Stress: Can weaken your immune system and compromise healing.
- Heart disease: Research shows a notable link between gum disease and heart health.
Diagnosis: What to Expect
A dentist or periodontist can diagnose periodontal disease during a routine exam. They’ll look for plaque buildup, gum inflammation and measure the depth of pockets around your teeth using a specialised probe. Dental X-rays can reveal areas of bone loss, helping your dentist determine the stage of gum disease.
Treatment Options for Periodontal Disease
Though gum disease isn’t always curable (especially in the advanced stages), effective treatment can halt or slow its progression. Your treatment plan depends on how severe the condition is and may include:
- Routine Dental Cleaning and Improved Oral Hygiene: Effective for gingivitis and early stages of gum disease. Maintaining a consistent brushing and flossing routine can reverse early gum inflammation.
- Scaling and Root Planing: A deep-cleaning approach to remove plaque and tartar below the gum line. The tooth roots are then smoothed to deter bacterial growth. Typically requires local anaesthesia.
- Pocket Reduction Surgery (Osseous Surgery): In moderate or advanced cases, the periodontist creates a small flap in your gums to clean deep pockets of plaque and tartar. Gums are then repositioned and sutured.
- Laser-Assisted Treatment (LANAP): Some practices use laser technology to target diseased tissue while preserving healthy gum tissue. It’s considered a less invasive alternative to traditional pocket reduction surgery.
- Bone Grafting and Guided Tissue Regeneration (GTR): Helps restore lost bone. Bone-grafting material is placed where bone has eroded, and a membrane can prevent soft tissue from encroaching, giving new bone the opportunity to grow.
- Gum Grafting (Tissue Graft): When gum recession is significant, tissue (often from the roof of your mouth) is grafted over exposed tooth roots to protect them and improve the gum line.
- Platelet-Rich Fibrin (PRF) or Platelet-Rich Plasma (PRP): Uses a small sample of your blood to collect growth factors that aid healing after periodontal surgery, potentially reducing recovery time and discomfort.
Prevention: How to Keep Your Gums Healthy
You can prevent most cases of gum disease with strong oral hygiene habits. Some people with genetic predispositions or existing health issues may require extra care. Key prevention strategies include:
- Brushing two to three times a day using fluoride toothpaste.
- Flossing daily to remove debris where your toothbrush can’t reach.
- Using an antibacterial or antimicrobial mouthwash to reduce plaque.
- Avoiding or quitting smoking and tobacco products.
- Visiting your dentist or periodontist for regular check-ups and cleanings.
- Managing underlying health conditions, such as diabetes.
Complications and Overall Health
Untreated periodontal disease can escalate, leading to tooth loss and widespread infection. Furthermore, evidence suggests a link between gum disease and health concerns like heart disease, stroke and diabetes. By treating gum disease early, you can help protect your teeth and potentially reduce risks related to your overall health.
Frequently Asked Questions
- Is gum disease contagious? Bacteria that lead to gum disease can be transferred through saliva, but passing the condition itself is less likely without prolonged close contact.
- Can I reverse periodontal disease? You can reverse gingivitis (the earliest stage) through professional cleaning and excellent home care. More advanced stages can be managed but aren’t fully reversible if bone loss has occurred.
- How long can I keep my teeth if I have periodontal disease? It depends on the progression and how quickly you seek treatment. Many people manage to keep their teeth by adhering to a consistent dental care routine and following professional advice.
- When should I see a dentist? If you notice signs like bleeding, swollen gums or persistent bad breath, book an appointment as soon as possible. Early intervention provides the best chance to prevent serious damage.
Outlook
While gum disease isn’t life-threatening, its impact on your oral health can be significant. Fortunately, with timely diagnosis, advanced treatments and careful home care, you can preserve your teeth and minimise complications. If you experience any gum discomfort, bleeding or sensitivity, don’t wait — contact your dentist or periodontist for personalised advice and treatment options.
Take Charge of Your Gum Health
Periodontal disease can be a hidden danger, gradually destroying the structures that support your teeth. Staying vigilant about your oral hygiene, attending regular dental check-ups and taking early action against gum disease are the best ways to safeguard your smile — and your overall health.
Emergency Dental Appointments Available in Neutral Bay
If you are in need an emergency dentist in the Lower North Shore we are here to help. Here at Elite Dentistry in Neutral Bay, we do all we can to ensure that any urgent dental problems are dealt with quickly and efficiently. This applies regardless of whether you are an existing patient or a new patient.
Our emergency dentists are available during clinic hours to meet urgent dental needs. We can offer same day appointments for knocked out teeth, dental pain, toothache, broken filings, lost crowns, root canal pain at our Neutral Bay dental practice. Dental emergencies can be very painful, so we do all we can to provide emergency dental services promptly, as we know dental traumas can arrive any moment.
Website & Mobile Development
What types of emergency dental treatment do we offer Neutral Bay dental practice?
- Severe toothaches
- Chipped or broken tooth
- Knocked-out tooth
- Partially dislodged tooth
- Lost filling
- Lost crown
- Trapped object between teeth
- Braces repair and removal caused by broken braces or wires
- Loose brackets and bands
- Gum abscesses and swollen gums
- Soft tissue injuries
- Emergency root canal treatments
- Emergency restorative services
Arrange
an appointment
right now
Start the process of achieving a better smile today by arranging an appointment. Just call us or if out of hours use our simple request a callback from and we will call you back when we are open.
Call 02 8350 5840
Arrange
an Appointment
Right Now
Start the process of achieving a better smile today by arranging an appointment. Just call us or if out of hours use our simple request a callback from and we will call you back when we are open.

